Before birth, most babies are in a head-down position in the mother’s womb. When the babies are bottom-first this is called a breech presentation. This occurs in about 5 % of pregnancies after 37 weeks. More complications can occur if the baby is delivered as a breech compared to a baby in the head-down position.
You have been advised to have the procedure (ECV) to try to turn the baby you are expecting, into this ‘head downwards’ position. Attempting an ECV lowers your chances of having a caesarean section (RCOG 2017)
For this procedure, you will be seen on the Delivery Suite, after 36 weeks into your pregnancy.
The procedure itself will last about 15 minutes. However, you can expect to be in hospital for two hours, which includes us monitoring the baby’s heart rate.
Before the procedure
- The procedure will be performed by a consultant obstetrician or registrar trained in performing an external cephalic version.
- You can discuss any concerns about the procedure with the staff present.
- If you are taking any tablets or other forms of medication, you should tell the doctor who is treating you.
- You can have a light breakfast and have clear fluids until the procedure.
During the procedure
It may be necessary to administer an injection to you prior to the commencement of the procedure. This helps to relax the uterus, which assists the doctor with the procedure. Your baby’s heart rate will be monitored using a continuous cardiotocograph for approximately 20-30 minutes to ensure there is no deviation from normal. If all is well, you will have an ultrasound scan to confirm the baby’s position.
While you are lying flat on the bed, the obstetrician will place his/her hands on your abdomen moving the baby up and out of the pelvis. The baby is turned either forward or backward until the baby is in the head-down position. You will then have another ultrasound to confirm the new position. We will also carry out another heart rate trace of the baby for 20-30 minutes.
After the procedure
When a baby is turned, there is a possibility that some of the baby’s blood will be transferred to the mother, which can sensitise her to the baby’s blood cells, which in turn, can affect subsequent pregnancies. For this reason, if the mother’s blood group is rhesus negative, an injection of ‘Anti D’ will be given at the end of the procedure. Your doctor or midwife can explain this in more detail.
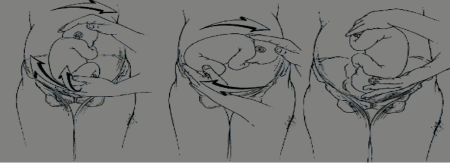
Image reproduced from Fandio, E., & Delgado Herrero, J. C. (2012). The External Version in Modern Obstetrics. Sifakis, S. & Vrachnis, N. (Eds.). From Preconception to Postpartum. InTech. Fig 2. https://
Alternative options
- A mother may choose to continue the pregnancy with the baby in the breech (bottom down) position and opt for vaginal breech delivery.
- An elective Caesarean section.
Frequently occurring risks
An external cephalic version is a very safe procedure; however, in common with all procedures there are potential risks involved.
The main risks of the procedure are:
- The baby can turn back to the breech position after this procedure.
- There is bleeding behind the placenta, which might require delivery of the baby by Caesarean section, and this is extremely rare;
- Rupture of the membranes may occur.
- There is immediate or delayed foetal distress, which can require delivery.
- Your obstetrician and midwife will ensure that the appropriate measures are taken to reduce your risk of the development of complications.
- Breech baby at the end of pregnancy | RCOG (Please use this link in your browser to access the RCOG leaflet)
George Eliot Hospital is a smoke free environment. For help and advice to stop smoking you can call the national helpline on 0300 123 1044 or https://
Copyright
Except where otherwise noted, this item is licensed under the CC BY license (https://
If you are a rights holder and are concerned that you have found material on our patient information resources website, for which you have not given permission, or is not covered by a limitation or exception in national law, please contact us using the Feedback form providing your contact information and full details of the material.