CT scan
Most people have a CT (computerised tomography) scan. If you have certain symptoms, you might have a CT scan, even if your chest x-ray is normal.
A CT scan makes a three-dimensional (3D) picture of the inside of the body using x-rays taken by the CT scanner. It uses a small amount of radiation. This is very unlikely to harm you and it will not harm anyone who you come into contact with. You will receive an appointment letter telling you if you need to do anything before the scan. You may be asked not to eat or drink for a few hours before the scan or other instructions. If this is a problem for you, call the number on your appointment letter.
You have the scan at the 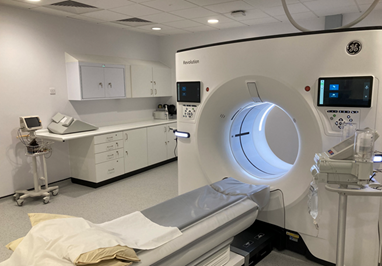
The contrast may make you feel hot all over for a few minutes. It is important to let your doctor know if you are allergic to iodine or have asthma. This is because you could have a more serious reaction.
You may be required to have a blood test to check your kidney function before you have the scan. This enables us to give you a contrast dye during the scan. You will be provided with the blood form for the kidney function check if this is required.
If you experience any difficulty in booking a blood test the Lung CNS (clinical nurse specialist) will be able to assist you.
The scan takes 5 to 10 minutes, but you may be in the department for longer. You will lie very still on a narrow bed. The bed moves slowly back and forward through the donut‑shaped scanner.
MRI scan
An MRI scan uses magnetism to build up a detailed picture of areas of your body. The scanner is a powerful magnet. You will be asked to complete and sign a checklist to make sure it is safe for you. The checklist asks about any metal implants you may have, such as a pacemaker or surgical clips. You should also tell your doctor if you have ever worked with metal or in the metal industry. Tiny fragments of metal can sometimes lodge in the body. You have the scan in the x-ray department at the hospital. A person called a radiographer works the scanner. They may give you an injection of a dye, called a contrast. It helps show certain areas of the body more clearly. During the test, you need to lie very still on a bed inside a long cylinder (tube). 
Breathing tests

• breathing tests (lung-function tests)
• exercise tests.
PET-CT scan
This is a combination of a CT scan and a PET (positron emission tomography) scan. A PET scan uses a glucose radiotracer to measure the activity of cells in different parts of the body. PET-CT scans give more detailed information about the part of the body being scanned.
This type of scan may be done instead of a CT scan. It can provide information to help your doctors plan your treatment. You cannot eat for 6 hours before the scan, although you may be able to drink. If you are a diabetic, you will be given specific instructions on how to manage this.
About an hour before the scan, the radiographer will inject a mildly radioactive sugar into a vein, usually in the arm. This is called a tracer. The scan itself usually takes 30 to 90 minutes but be prepared to be there for several hours. PET-CT scanners are not available at George Eliot Hospital, and you will be required to travel to University Hospitals Coventry and Warwickshire (UHCW).
Biopsy
You may require a tissue biopsy to find out the cause of the changes/abnormalities seen. A doctor takes samples of cells or tissue from the abnormal area. They look at the biopsy samples under a microscope to check for its characteristics.
There are different ways of doing a biopsy. Your doctor or nurse will talk to you about the type of biopsy you will have.
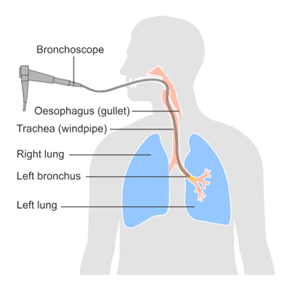
Bronchoscopy biopsy
A doctor uses a thin, flexible tube (bronchoscope) to look inside your airways and lungs. The tube has a tiny camera on the end. The camera shows a picture of the area on a screen. They can take samples of cells (biopsies) from your lung or airways using the bronchoscope.
Before the test, you should not eat or drink anything for a few hours. The doctor gives you a sedative to help you relax. They also spray a local anaesthetic onto the back of your throat to numb it. After this, they pass the bronchoscope through your nose or mouth and down into your windpipe (trachea). A bronchoscopy usually takes up to 30 minutes. Afterwards, you should not eat or drink for at least 1 hour. You can go home as soon as the sedation has worn off. You cannot drive for 24 hours after the sedation. You may have a sore throat for a couple of days.
Endobronchial ultrasound scan (EBUS)
Some people have an EBUS to help obtain a diagnosis. An EBUS lets the doctor look into the lungs through the walls of the airways. They use an ultrasound to see the area. An ultrasound uses soundwaves to produce a picture. The doctor takes biopsy samples of the lymph nodes in the centre of your chest.
The doctor will pass a thin, flexible tube (bronchoscope) through your mouth into your windpipe (trachea). It has a tiny camera and ultrasound on the end which shows a picture of the area on a screen. The doctor passes a needle through the wall of the airway and takes samples (biopsies) of the lung and lymph nodes. An EBUS takes less than an hour. You will go home on the same day unless unforeseen complications have arisen.
Endoscopic ultrasound (EUS)
This is like an EBUS. A EUS takes a biopsy from the lymph nodes in the middle of the chest. But the doctor does this by passing a small, flexible tube (endoscope) through your mouth and into your gullet (oesophagus). The gullet is behind your windpipe and close to lymph nodes in the chest. The doctor passes a thin needle along the endoscope to take biopsies from the lymph nodes. This type of procedure would be undertaken at UHCW.
CT scan/ultrasound and biopsy
CT scans and ultrasound scans can be used to guide a biopsy. You can usually have this as a day patient but please do expect to be at the hospital for half a day.
Lung biopsy through the skin: Using CT scanner or ultrasound machine.
You usually have this test during a CT scan/ultrasound. This helps the doctor find the exact area to take the biopsy from. It is sometimes called a percutaneous biopsy. Your doctor gives you an injection of local anaesthetic into the skin to numb the area. They pass a thin needle through the skin (percutaneous) into your lung and take the biopsy. You may feel a pushing sensation, but it only takes a few minutes. After the biopsy, you stay in hospital for a few hours to make sure there are no problems. You will also have a chest x-ray, because there is a small risk of air getting into the space between the pleura. If this happens, it can make the lung collapse (pneumothorax). The treatment of this is dependent upon the size of the air leak and sometimes you may need to come into hospital for this to be managed effectively.
Biopsy of neck lymph nodes
Sometimes the doctor takes a sample of cells from the lymph nodes in the neck. They use an ultrasound scan to examine the lymph nodes. The doctor passes a thin needle into a lymph node and takes a sample of cells. You can have this test as an outpatient and go home on the same day.
Mediastinoscopy
This is sometimes done instead of an EBUS or EUS. It lets the doctor look at the area in the middle of your chest (the mediastinum) and nearby lymph nodes. You have it under a general anaesthetic. You may need to stay overnight in hospital to have it done. The doctor makes a small cut in the skin at the base of your neck. They pass a thin, flexible tube with a tiny camera on the end through the cut into your chest. It shows a picture of the area on a screen. Your doctor can take a biopsy of the tissue and lymph nodes in the area. This procedure would be undertaken at UHCW.
Thoracoscopy (Can be medical or surgical).
This lets the doctor look at the lining of the lungs (pleura). It is usually done under a general anaesthetic for a surgical thoracoscopy at UHCW or sedation for a medical thoracoscopy at GEH. The doctor makes one or two small cuts in your chest. They pass a thin, flexible tube called a thoracoscope into your chest through a cut and take a biopsy of the pleura. They can also remove any fluid that may have collected there.
Following this procedure, you will be admitted to hospital for several days.
Video-assisted thoracoscopy
Sometimes the surgeon attaches a video camera to the thoracoscope. This lets them see the area more clearly.
Anticoagulation
If you are prescribed an anticoagulant (blood thinning medication) please let the team know so they can advise if this medication needs to be stopped before a biopsy/procedure.
Waiting for test results
We appreciate that waiting for test results can be a difficult time. It may take several weeks for all the results to be available and for your case to be discussed at our specialist Multi-Disciplinary Team meeting. Your lung CNS is there to support you through these investigations and whilst awaiting results and can be contacted on 02476153247.
Please note this is a brief overview and you will be given more in-depth information and a chance to ask any questions when your procedures have been determined.
This information is adapted from content originally produced by Macmillan Cancer Support, reused with permission.
George Eliot Hospital is a smoke free environment. For help and advice to stop smoking you can call the national helpline on 0300 123 1044 or visit https://
Copyright:
Endobronchial ultrasound scan (EBUS) Image credit: © Cancer Research UK [2002] All rights reserved. Information taken 27/12/2023.
Except where otherwise noted, this item is licensed under the CC BY license (https://
If you are a rights holder and are concerned that you have found material on our patient information resources website, for which you have not given permission, or is not covered by a limitation or exception in national law, please contact us using the Feedback form providing your contact information and full details of the material.