Our work to Reduce Health Inequalities
Everyone deserves fair healthcare and we aim to provide that – no matter who you are, where you live or your personal circumstances.
Our trust works to understand the complex health needs of our communities so that we can plan interventions to meet needs, prioritise areas for development, to improve population health and reduce health inequalities. Our work looks to identify how the onset of disease, treatment and outcomes of disease vary across our patients and take steps to reduce this variation, improving health for all.
While your physical health is very important, we know that your mental wellbeing and social life plays a part in your health too. So, while we may be looking after you for medical reasons, we will always look at your health as a whole and consider the many factors, often referred to as social determinants of health, that can affect you in your life. These include who you are – your age, gender and genetics – and your behaviours that can affect your health such as smoking, how active you are, how much alcohol you drink and what you eat.
What are Healthcare Inequalities?
Health inequalities are unfair and avoidable differences in health across the population, and between different groups within society. These include how long people are likely to live, the health conditions they may experience and the care that is available to them.
The conditions in which we are born, grow, live, work and age can impact our health and wellbeing. These are sometimes referred to as wider determinants of health.
Wider determinants of health are often interlinked. For example, someone who is unemployed may be more likely to live in poorer quality housing with less access to green space and less access to fresh, healthy food. This means some groups and communities are more likely to experience poorer health than the general population. These groups are also more likely to experience challenges in accessing care.
The reasons for this are complex and may include:
- the availability of services in their local area
- service opening times
- access to transport
- access to childcare
- language (spoken and written)
- literacy
- poor experiences in the past
- misinformation
- fear
People living in areas of high deprivation, those from Black, Asian and minority ethnic communities and those from inclusion health group, for example the homeless, are most at risk of experiencing these inequalities.
COVID-19 has shone a harsh light on some of the health and wider inequalities that persist in our society. Guidance issued by NHS England in response to the COVID-19 pandemic, set out eight urgent actions for tackling health inequalities. This was later refined to five key priority areas which underpin the work of the National Healthcare Inequalities Improvement Programme.
We have also developed our Core20Plus5 approach to support the reduction of healthcare inequalities.
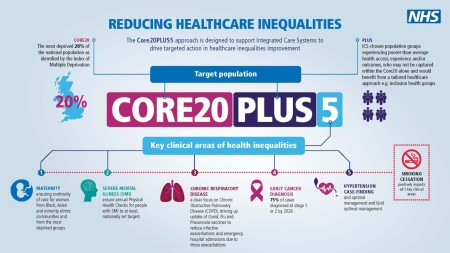
The approach, which initially focussed on healthcare inequalities experienced by adults, has now been adapted to apply to children and young people.
The information below outlines the Core20PLUS5 approach for adults.
Core20
The most deprived 20% of the national population as identified by the national Index of Multiple Deprivation (IMD). The IMD has seven domains with indicators accounting for a wide range of social determinants of health.
PLUS
PLUS population groups should be identified at a local level. Populations we would expect to see identified are ethnic minority communities; people with a learning disability and autistic people; people with multiple long-term health conditions; other groups that share protected characteristics as defined by the Equality Act 2010; groups experiencing social exclusion, known as inclusion health groups coastal communities (where there may be small areas of high deprivation hidden amongst relative affluence).
Inclusion health groups include: people experiencing homelessness, drug and alcohol dependence, vulnerable migrants, Gypsy, Roma and Traveller communities, sex workers, people in contact with the justice system, victims of modern slavery and other socially excluded groups.
5
There are five clinical areas of focus which require accelerated improvement. Governance for these five focus areas sits with national programmes; national and regional teams coordinate activity across local systems to achieve national aims.
1. Maternity
Ensuring continuity of care for women from Black, Asian and minority ethnic communities and from the most deprived groups. This model of care requires appropriate staffing levels to be implemented safely.
2. Severe mental illness (SMI)
Ensure annual physical health checks for people with SMI to at least nationally set targets.
3. Chronic respiratory disease
A clear focus on Chronic Obstructive Pulmonary Disease (COPD) driving up uptake of COVID, flu and pneumonia vaccines to reduce infective exacerbations and emergency hospital admissions due to those exacerbations.
4. Early cancer diagnosis
75% of cases diagnosed at stage 1 or 2 by 2028.
5. Hypertension case-finding and optimal management and lipid optimal management
To allow for interventions to optimise blood pressure and minimise the risk of myocardial infarction and stroke.
Please see the supporting document for further information.
See below some of the projects in place to help improve access to healthcare.
Heart Failure Nursing Service
Street Outreach Team
Community Heart Health Checks
Patient Information Resources